Introduction: Appointment notes are a fundamental aspect of maintaining comprehensive medical records in Embark EMR. These notes are automatically generated when an appointment is scheduled and can be accessed and edited through the Schedule or the Client’s Profile. This guide provides a step-by-step approach to using the Appointment Note feature effectively.
Accessing and Editing Appointment Notes: To access an appointment note, navigate to either the Schedule or the Client’s Profile. Locate the desired appointment and click the “Edit Note” button to open the note for editing.
Key Sections of the Appointment Note:
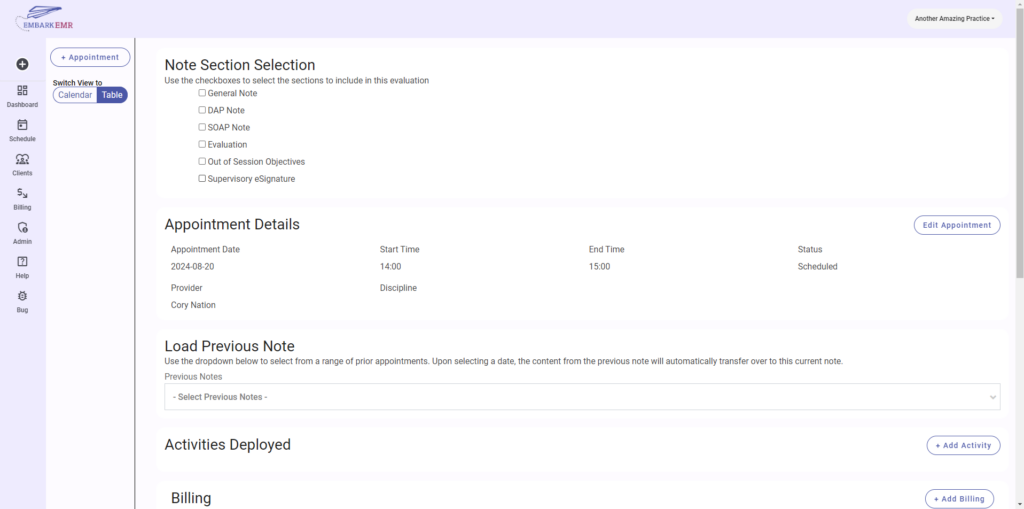
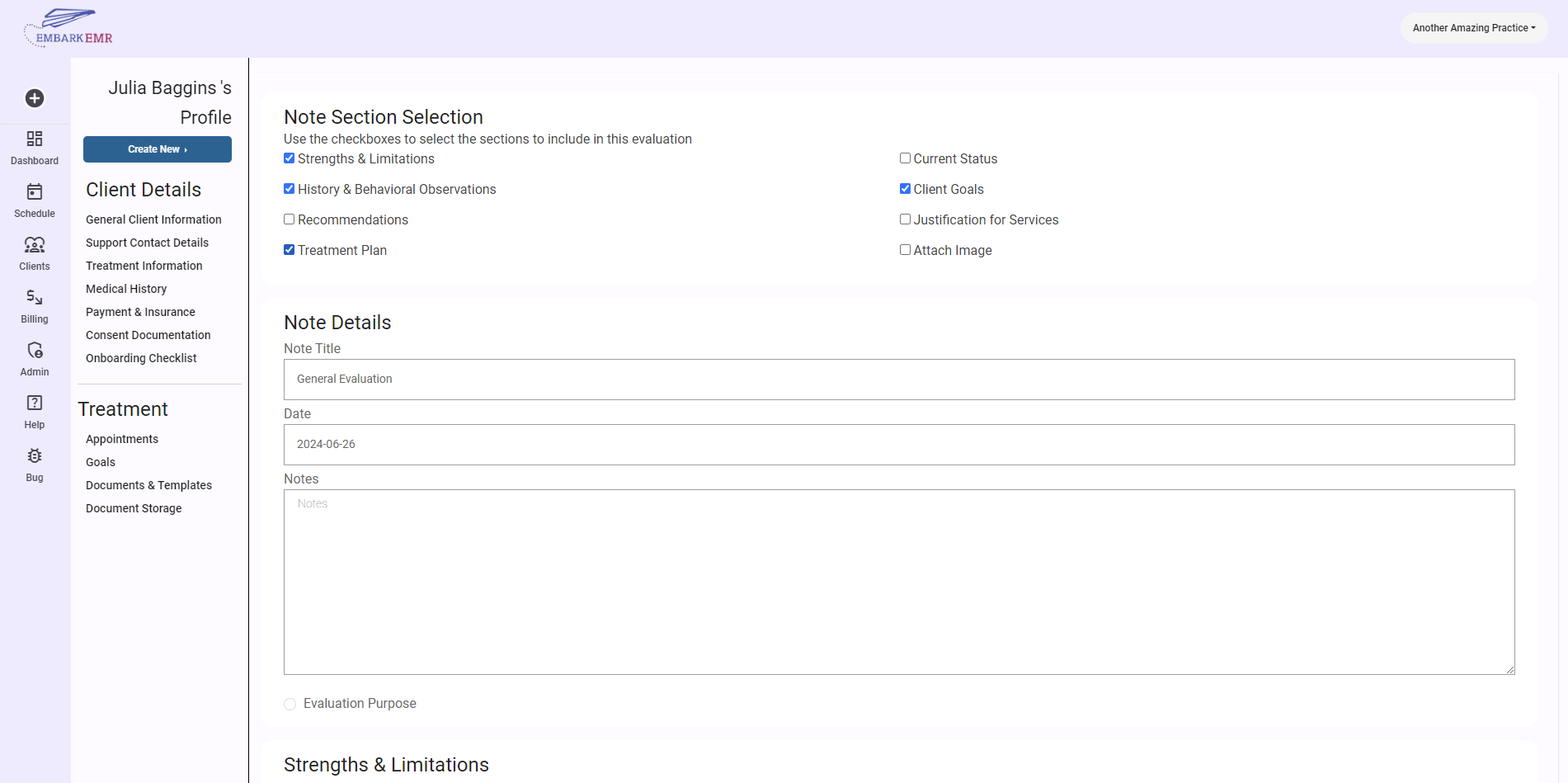
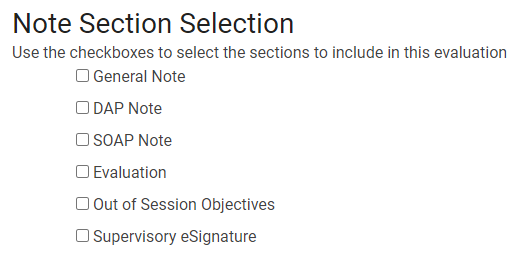
Note Section Selection:
- This section allows you to customize the structure of your appointment note by selecting the desired elements. Customize your template by checking the boxes next to these options. Available options include
- General Note: A large flexible text box to enter a range of open text into.
- DAP Note (Data, Activity, Plan): Contains fields for Data, the ability to add activities to the note, and adjust the plan
- SOAP Note (Subjective, Objective, Assessment, Plan): Available are buttons and a text box for Subjective. Objective allows the user to add notes and add any activities compelted during session. Assessment contains an open text field and the ability to add client goals to the note from the client’s profile. Plan allows to continue/modify the plan of care and add notes.
- Evaluation: The Evaluation section is the same format as a SOAP note, however, instead of the Plan section, you are able to create a plan of care for the client.
- Out of session objectives: Any activities or homework assigned to the client for completion before the next appointment
- Supervisory eSignature: For unlicensed clinicians, it may be necessary to have a licensed clinitian review your notes. In this case, by checking this section, an additional signature line will appear at the bottom of the note for a supervisor to sign off on the note.
- This section allows you to customize the structure of your appointment note by selecting the desired elements. Customize your template by checking the boxes next to these options. Available options include
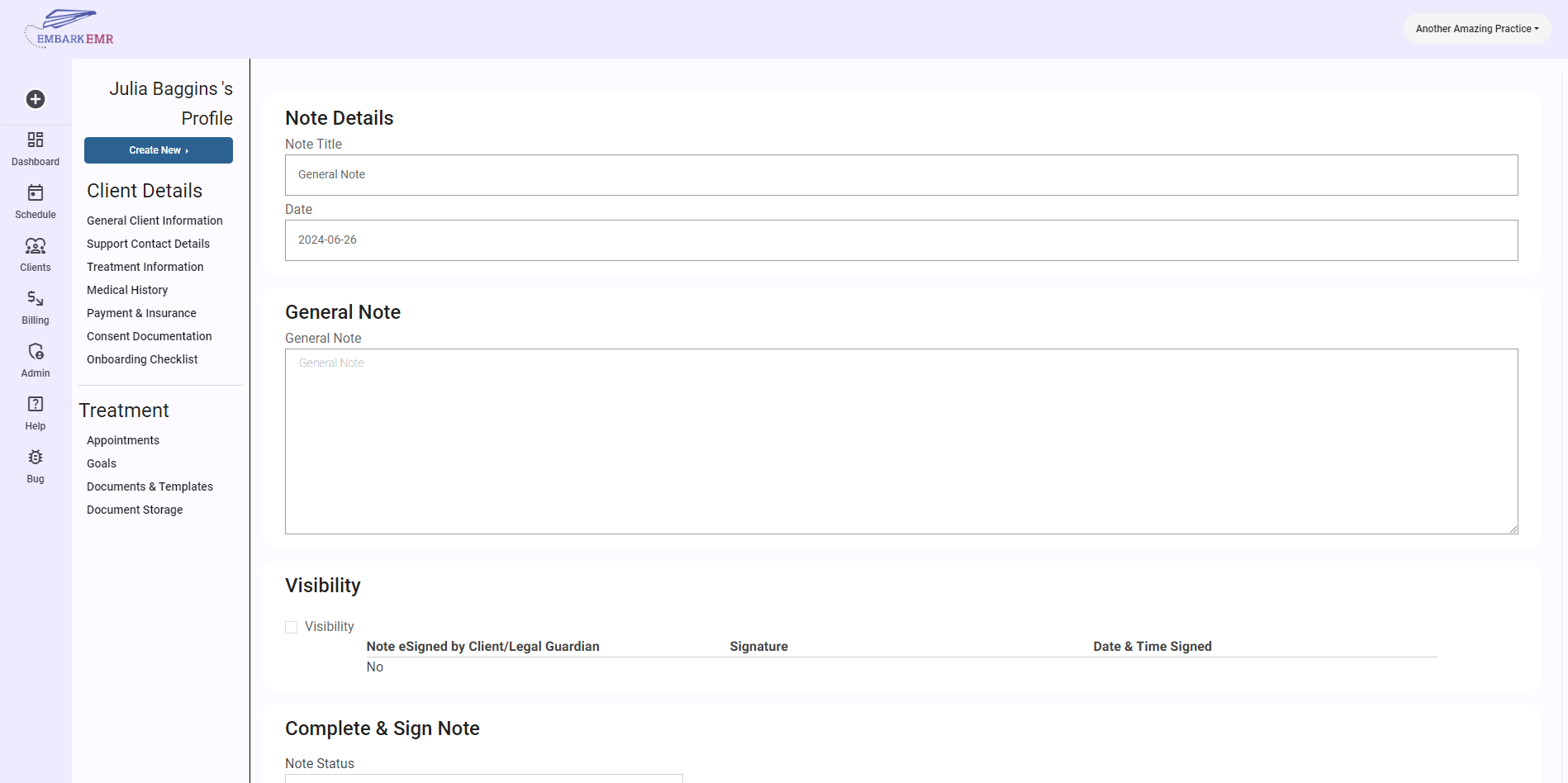
Note Body:
- The body of the note will dynamically update to display the sections you have selected, allowing you to fill in detailed information for each part.
- Adding Activities and Goals:
- When sections like DAP, SOAP, or Evaluation are included, additional details such as activities and goals related to the appointment can be added:
- Add Activity: Click the “+ Add Activity” button and fill in the fields in the form that appears, including Procedure, Activity, Repetition, and Comments.
- Add Goals: Click the “+ Add Goals” button to select a goal from the client’s active goals list, document progress, and assign a completion percentage based on the client’s performance during the session.
- When sections like DAP, SOAP, or Evaluation are included, additional details such as activities and goals related to the appointment can be added:
Billing:
- Since Embark EMR does not automatically know the services provided during an appointment, the Billing section is critical. Add services by clicking the “+ Add Billing” button and selecting the relevant services that were rendered during the appointment.
Visibility:
- By default, notes are hidden from clients. However, to comply with HIPAA requirements, you can easily make them accessible to clients by checking the boxes to Release Note to Client, Release Out of Session Objectives, and/or Request Client Signature.
Complete & Sign Note:
- Once all information is accurately entered, set the Note status to Complete (or sign-off needed), enter the date of completion, and add your eSignature along with your credentials to formally complete the note.
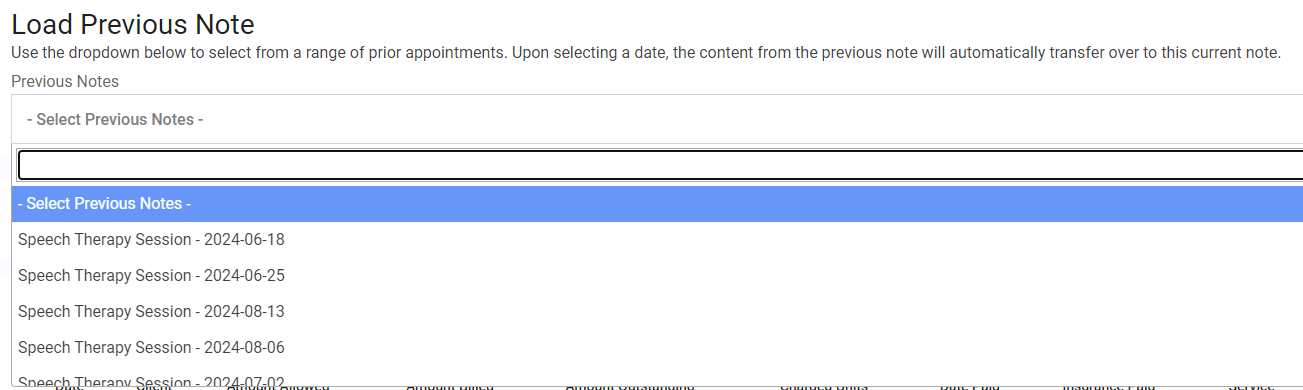
Utilizing the Load Previous Note Feature:
- To save time and maintain consistency, use the “Load Previous Note” option by selecting a date from the dropdown menu. This will copy the content from a previous note into the current note fields.
Saving the Note:
- After completing all necessary entries and reviews, ensure to click the “Update” button at the bottom of the page to save all changes and updates to the note.
Conclusion: The Appointment Note feature in Embark EMR is designed to streamline the documentation process, ensuring all pertinent information is accurately recorded and easily accessible. By following these guidelines, you can efficiently manage your appointment notes, enhancing both compliance and care quality.
Remember: Regularly updating and reviewing appointment notes is crucial for accurate record-keeping and effective patient management. Ensure your notes are detailed and compliant with all regulatory requirements to maximize the benefits of your EMR system.