Introduction:
Evaluation templates in Embark EMR are crucial tools for assessing a client’s health status, diagnosing conditions, and planning treatment strategies. These templates facilitate detailed examinations and ensure consistent documentation across visits. This article will guide you through the process of creating and using an Evaluation template within Embark EMR to enhance your clinical assessments.
Purpose of a Medical Evaluation:
Medical evaluations are systematic processes used by healthcare providers to assess and document a client’s current health status or progress over time. They involve reviewing the client’s medical history, conducting physical exams, and sometimes ordering diagnostic tests. The primary purposes of medical evaluations include:
- Diagnosis: Identifying diseases or conditions based on symptoms and test results.
- Baseline Establishment: Creating a baseline health profile for new clients or at the onset of a new treatment plan.
- Monitoring: Tracking the progress or changes in a client’s condition over time, particularly before and after interventions.
- Decision-Making: Informing treatment decisions, including modifications to ongoing plans based on the client’s response to treatment.
- Compliance and Documentation: Ensuring that all clinical assessments meet regulatory requirements and are properly documented for future reference and audits.
Creating an Evaluation Note:
Navigate to the Client’s Profile:
- Access the client’s profile by selecting their name or file from your client list.
Initiate Note Creation:
- Click the “Create New” button in the top left menu of the client’s profile and select the desired Evaluation template from the dropdown. Alternatively,
- Visit the “Documents & Templates” section and click “Add New.” Select the desired evaluation template from the dropdown menu.
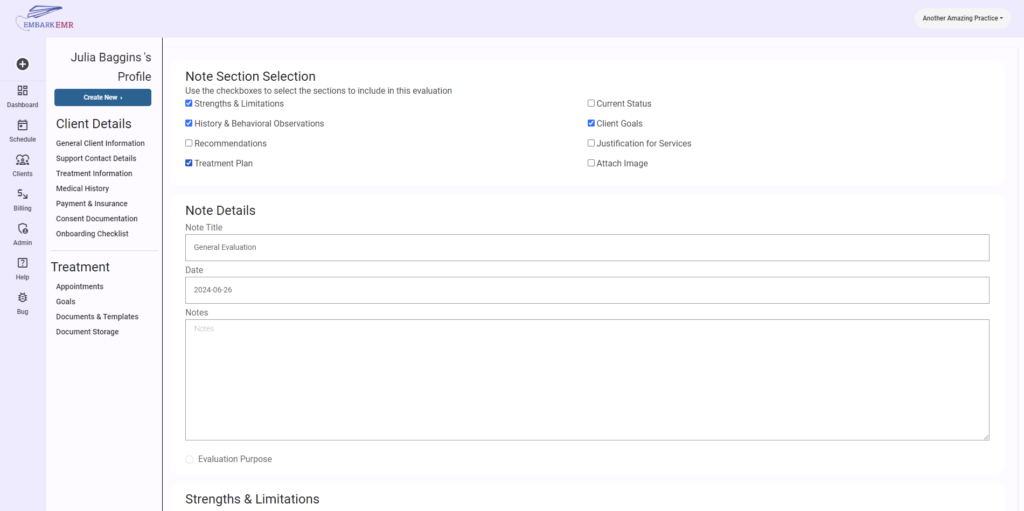
Configure the Evaluation Note:
- Set the date of the evaluation and provide a descriptive title that helps identify the note’s purpose and content.
- Click “Add” to create the note template, which will then be accessible from the “Documents & Templates” section.
Using the Evaluation Template:
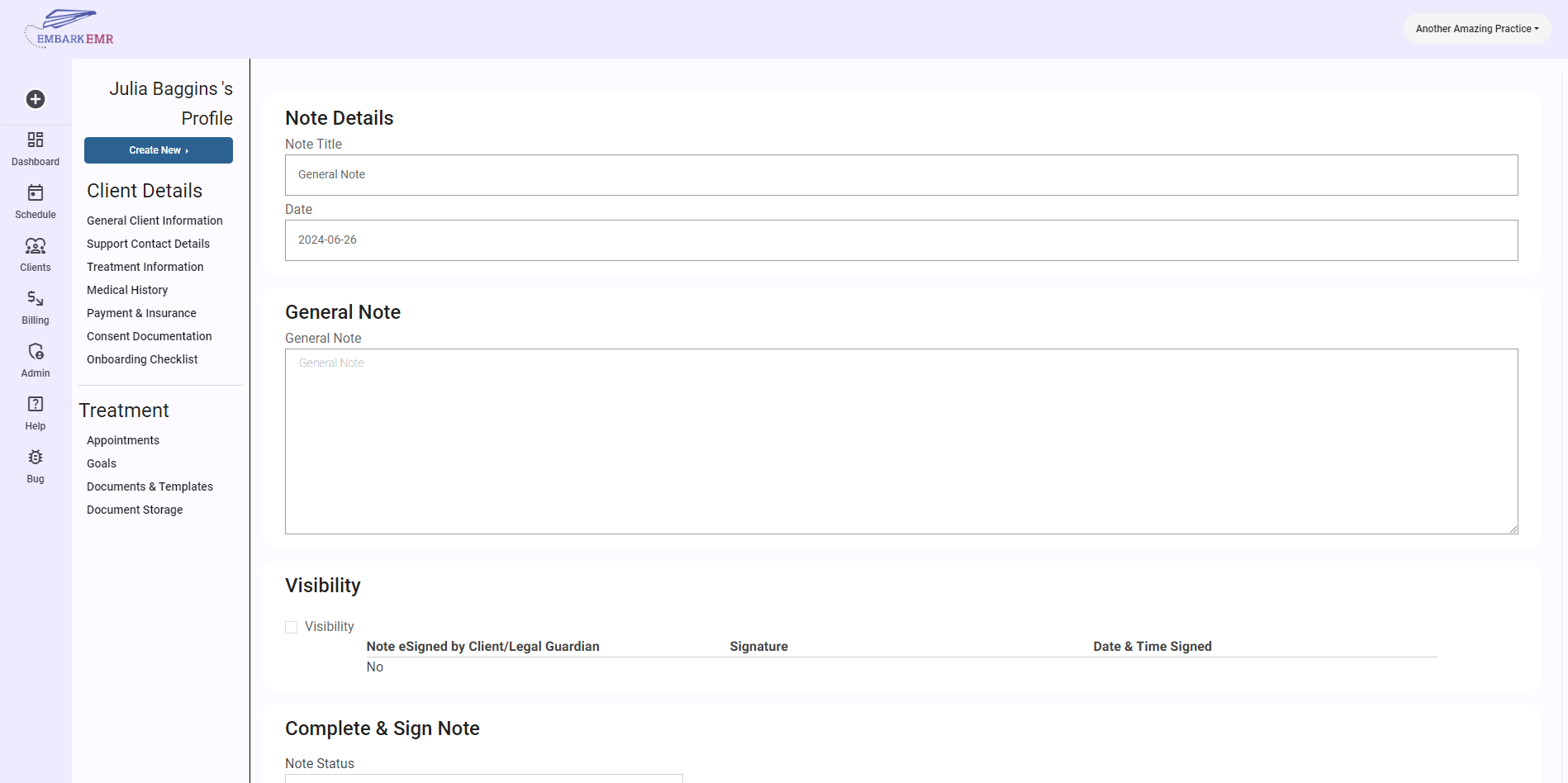
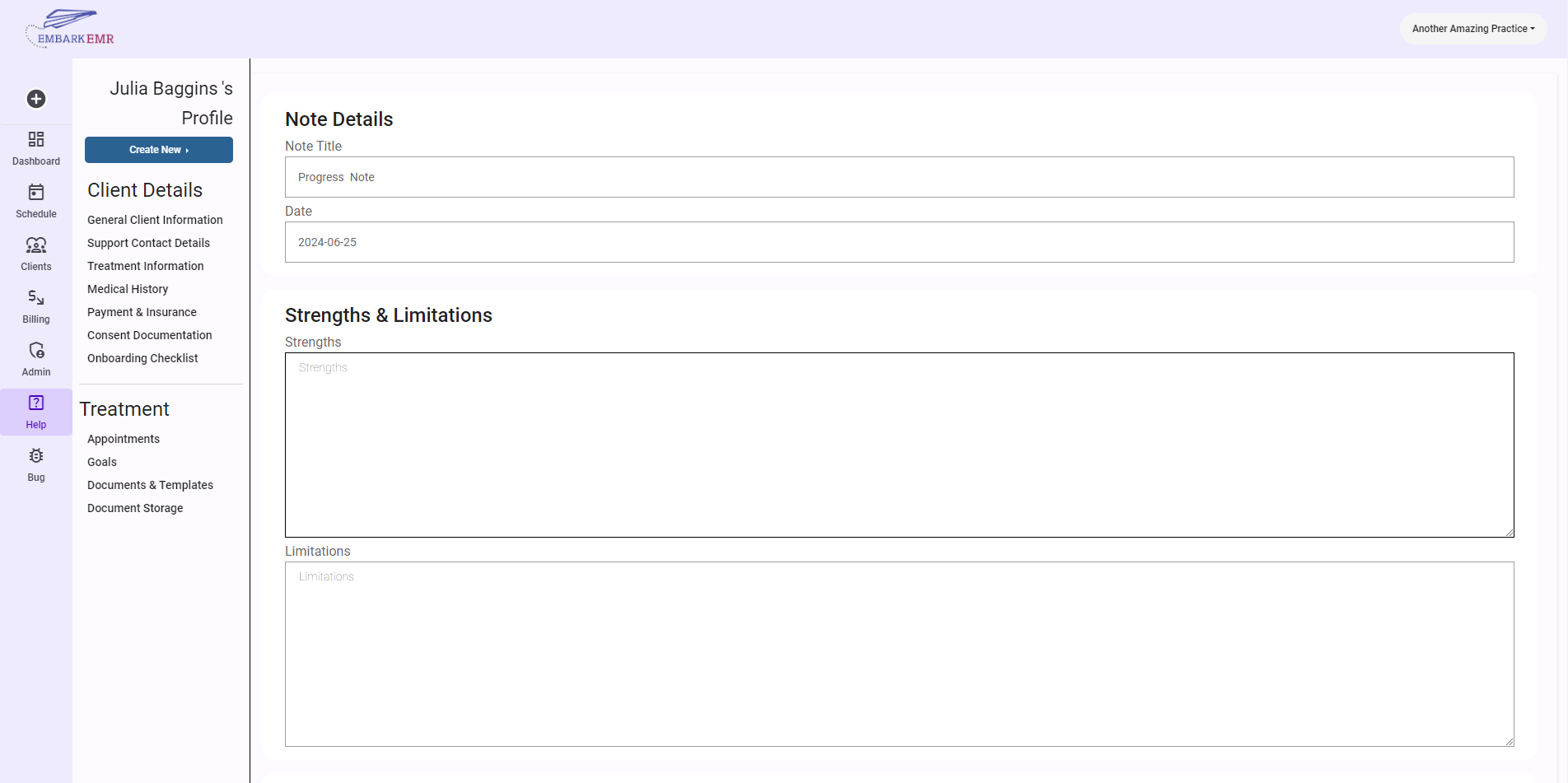
Document Findings:
- Fill out the evaluation template by entering data gathered during the client’s evaluation. This might include symptoms, test results, observations, and any other relevant information that supports your clinical decisions.
Share and Collaborate:
- If needed, share the note with the client through the client portal to enhance transparency and client engagement in their care process. This step may include requesting an electronic signature from the client to acknowledge their review and understanding of the evaluation.
Provider Verification:
- As a final step, the healthcare provider must electronically sign and date the note at the bottom. Ensure all information is accurate and complete before finalizing.
Save and Update:
- Click “Update” to save the evaluation note in the client’s electronic record, ensuring that all documentation is current and easily accessible.
Adding Client Goals to an Evaluation:
Integrating client goals into the evaluation process not only provides a structured framework for assessing progress but also aligns treatment plans with specific outcomes. This section of the evaluation note allows healthcare providers to create, manage, and track client goals directly within the evaluation, ensuring that these goals are both relevant and visible throughout the client’s care continuum.
Enable Client Goals:
- Within the evaluation note, locate the note index and check the “Client Goals” checkbox. This action will activate the goal-setting functionality within the document.
Create New Goals:
- Click the “Add Goals” button, which will open a dialogue box designed for goal creation. Fill out the following fields to define each new goal
- Goal Type: Select the nature of the goal: short-term, long-term, or if the field is not applicable. For short-term goals, you have the option to link the goal to an existing long-term goal, creating a cohesive treatment pathway
- Goal Status: Choose from Ongoing, Future Goal, Goal Met, or Discontinued to accurately reflect the current status of the goal. This helps in tracking progress and making necessary adjustments in the treatment plan.
- Goal Description: Provide a clear and concise description of what the client is expected to achieve. This description should be specific enough to guide therapeutic interventions and measurable to assess progress.
- Baseline: Document the client’s initial status related to the goal at the start of the evaluation period. This serves as a benchmark against which future progress will be measured.
- Intervention: Detail the therapeutic strategies or interventions planned to achieve the stated goal. This might include specific therapies, exercises, or other treatment modalities relevant to the client’s needs.
- Provider Notes: Include any additional observations, considerations, or instructions that may be useful for future reference or for other team members involved in the client’s care.
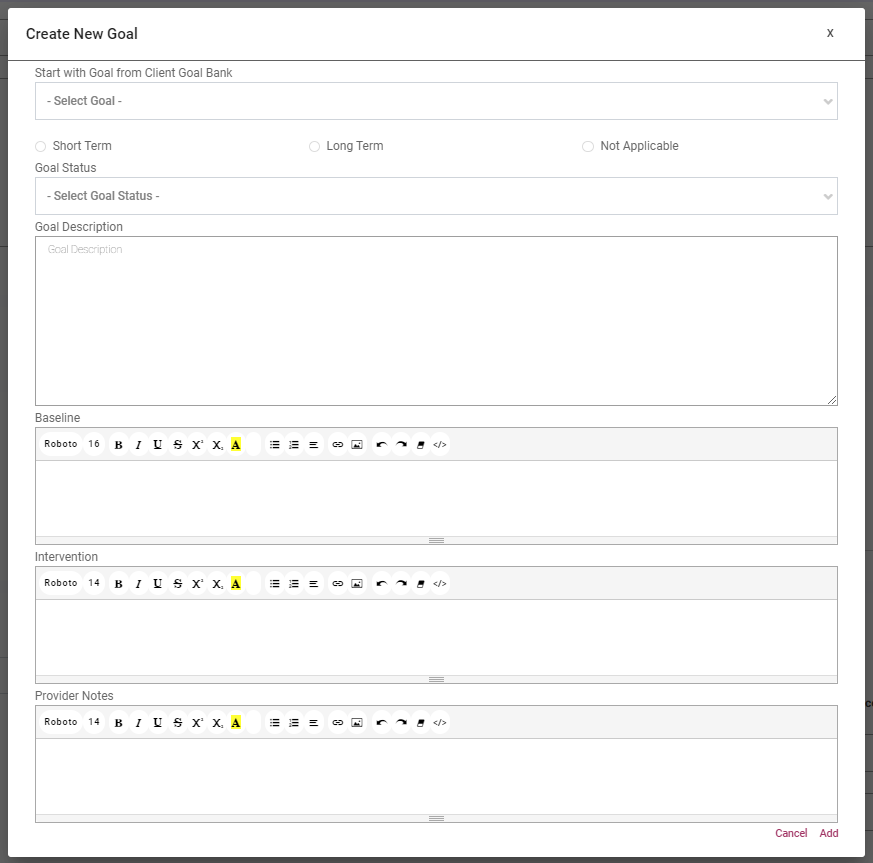
- Click the “Add Goals” button, which will open a dialogue box designed for goal creation. Fill out the following fields to define each new goal
Review and Save Goals:
- After filling out all necessary fields, review the information for accuracy and completeness. Once verified, save the goal, which will automatically add it to the evaluation note’s goal table and to the client’s profile under the “Client Goals” section.
Managing Goals Within the Evaluation:
- Within the evaluation note, each goal will be displayed in a dedicated table that includes all the information entered. This table serves as a quick reference for the provider during the evaluation and aids in discussing progress with the client.
- The goals saved during the evaluation will also update the “Client Goals” section of the client’s profile, ensuring continuity of care and easy access to historical goal data for all providers involved in the client’s care.
Requesting New Templates:
Embark EMR continuously updates its template library based on user feedback and the evolving needs of the healthcare community. If you require a new evaluation template that better suits your practice, please reach out to us with your suggestions at Info@EmbarkEMR.com.
Conclusion:
Evaluation templates are essential in providing structured and thorough assessments of client health. By utilizing these templates in Embark EMR, healthcare providers can ensure comprehensive care and accurate documentation, which are critical for effective treatment and client satisfaction.