Introduction:
The General Note template in Embark EMR offers a flexible and powerful tool for documentation when specific structured notes aren’t required. This template acts like a HIPAA-compliant word processor, allowing healthcare providers to freely format text and capture a wide range of information. This article will guide you through the steps to create, use, and manage a General Note within Embark EMR.
Creating a General Note:
Navigate to the Client’s Profile:
- Begin by accessing the profile of the client for whom you want to create a note.
Initiate Note Creation:
- Click the “Create New” button located in the top left menu of the client’s profile. From the dropdown, select “General Note.” Alternatively,
- You can also access this feature through the “Documents & Templates” section of the client’s profile by clicking the “Add New” button.
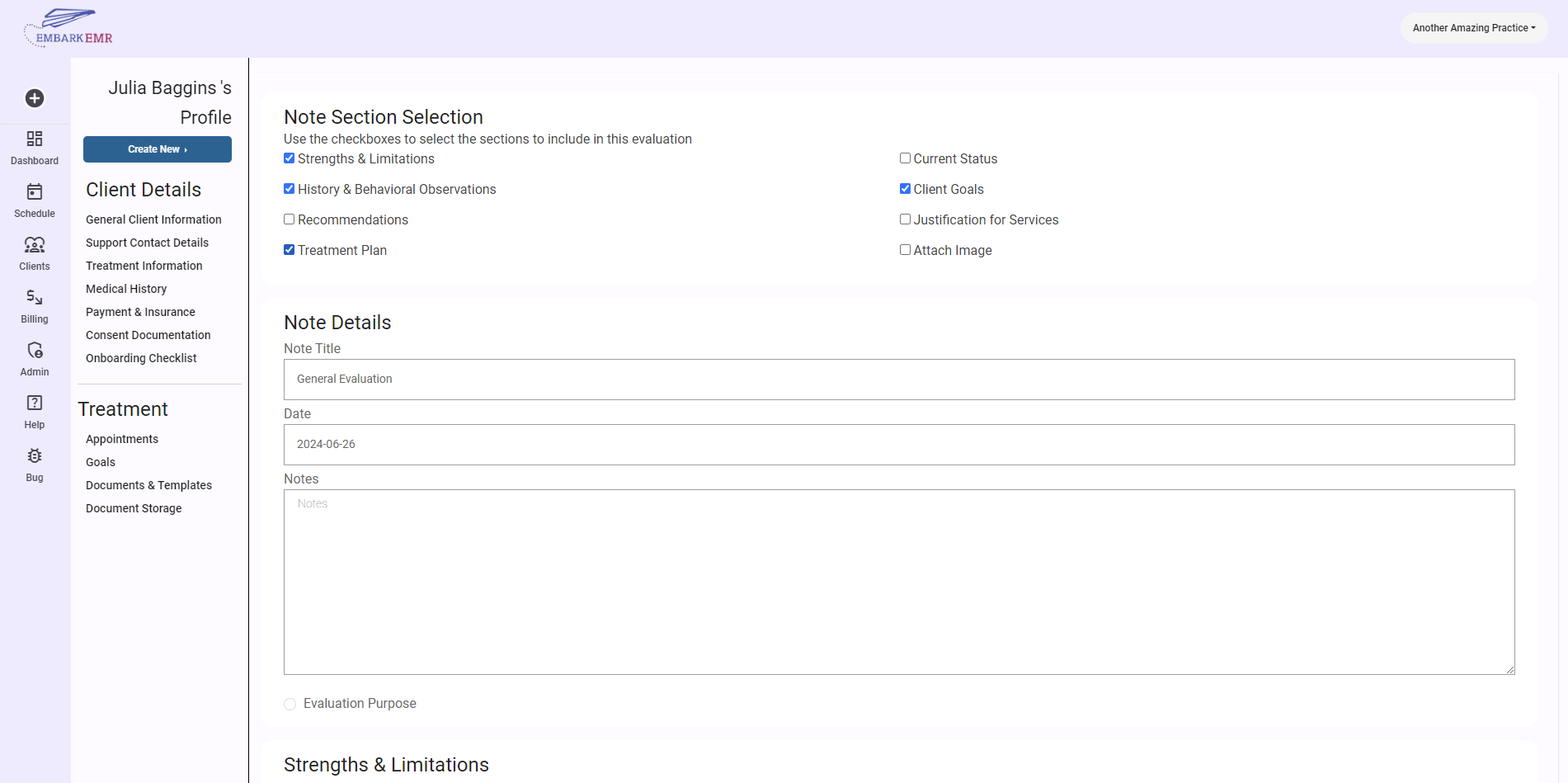
Configure the Note:
- Once the dialogue box appears, perform the following:
- Select Template: Choose “General Note” from the dropdown menu.
- Date: Specify the date for the note.
- Title: Provide a clear, descriptive title for the note.
- Click “Add” to create the note template, which will now be stored and accessible in the “Documents & Templates” section.
- Once the dialogue box appears, perform the following:
Using the General Note Template:
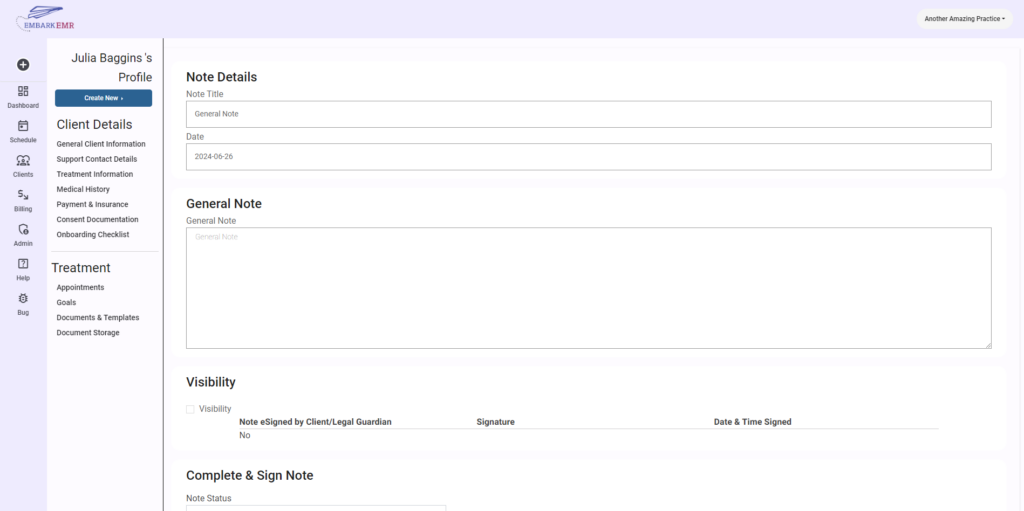
Access the Note:
- Navigate to the “Documents & Templates” section and select the General Note you created.
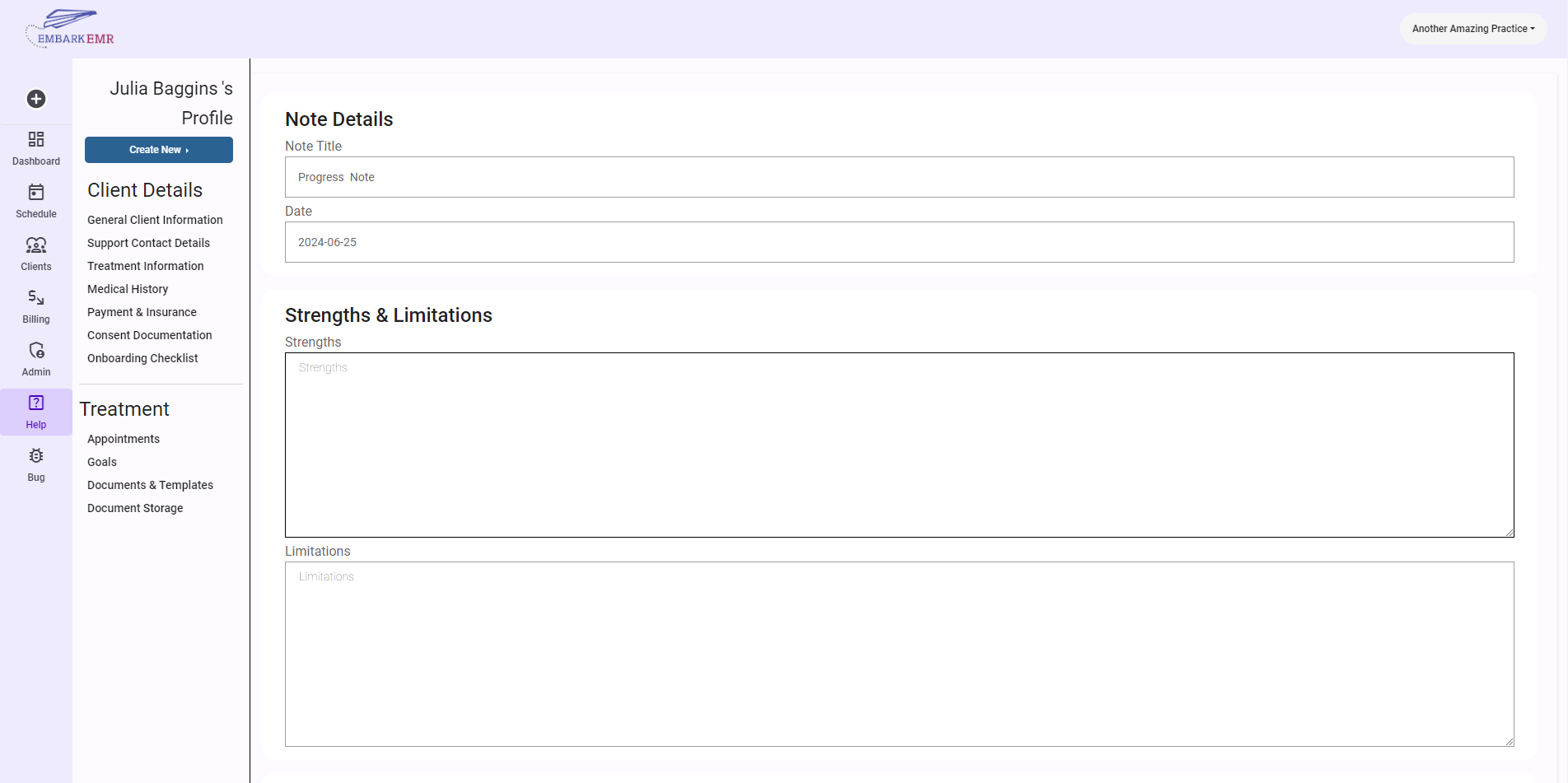
Compose the Note:
- The General Note template features a large text box where you can enter and format your text. Utilize this space to document any necessary information that doesn’t fit the structure of other specific templates.
- This flexible environment is ideal for detailed descriptions, narrative accounts, miscellaneous observations, or any other documentation that requires free-form text.
Sharing and Signing the Note:
- Release the Note to the Client: If you wish to make the note accessible to the client via the client portal, select the option to release the note to the client.
- Request Client E-Signature: You can also request an electronic signature from the client, which adds an extra layer of confirmation and engagement.
- Provider E-Signature: Before finalizing the note, ensure you sign and date it electronically at the bottom of the template to validate its contents.
Save Updates:
- Once all information is entered, and signatures are in place, click the “Update” button to save the changes and securely store the note in the client’s record.
Conclusion:
The General Note template in Embark EMR is a vital tool for situations where unstructured, detailed documentation is necessary. It provides the flexibility required to capture comprehensive and varied information in a secure, organized manner. By following these steps, healthcare providers can ensure that all pertinent data is effectively recorded and readily available for future reference.
Tip: Make frequent use of the formatting tools available within the General Note template to keep your documentation clear and well-organized. Regularly updating and reviewing notes to reflect the most current information will enhance the continuity and quality of care provided to your clients.