Introduction:
Progress and discharge notes are essential documents within any healthcare practice, providing a structured method for tracking a client’s journey towards their health goals and summarizing their care upon discharge. Embark EMR simplifies the creation and management of these notes, ensuring they are both comprehensive and accessible. This guide will walk you through the process of creating, filling out, and finalizing a progress/discharge note within Embark EMR.
Step-by-Step Guide to Creating a Progress/Discharge Note:
Access the Client’s Profile:
- Start by navigating to the desired client’s profile where you want to create the progress/discharge note.
Initiate Note Creation:
- From the Create New Button: Click the “Create New” button located in the top left menu of the client’s profile page. From the dropdown options, select “Progress/Discharge Note.” Alternatively,
- From the Documents & Templates Section: You can go to the “Documents & Templates” section of the client’s profile. Click the “Add New” button and select “Progress/Discharge Note” from the dropdown menu.
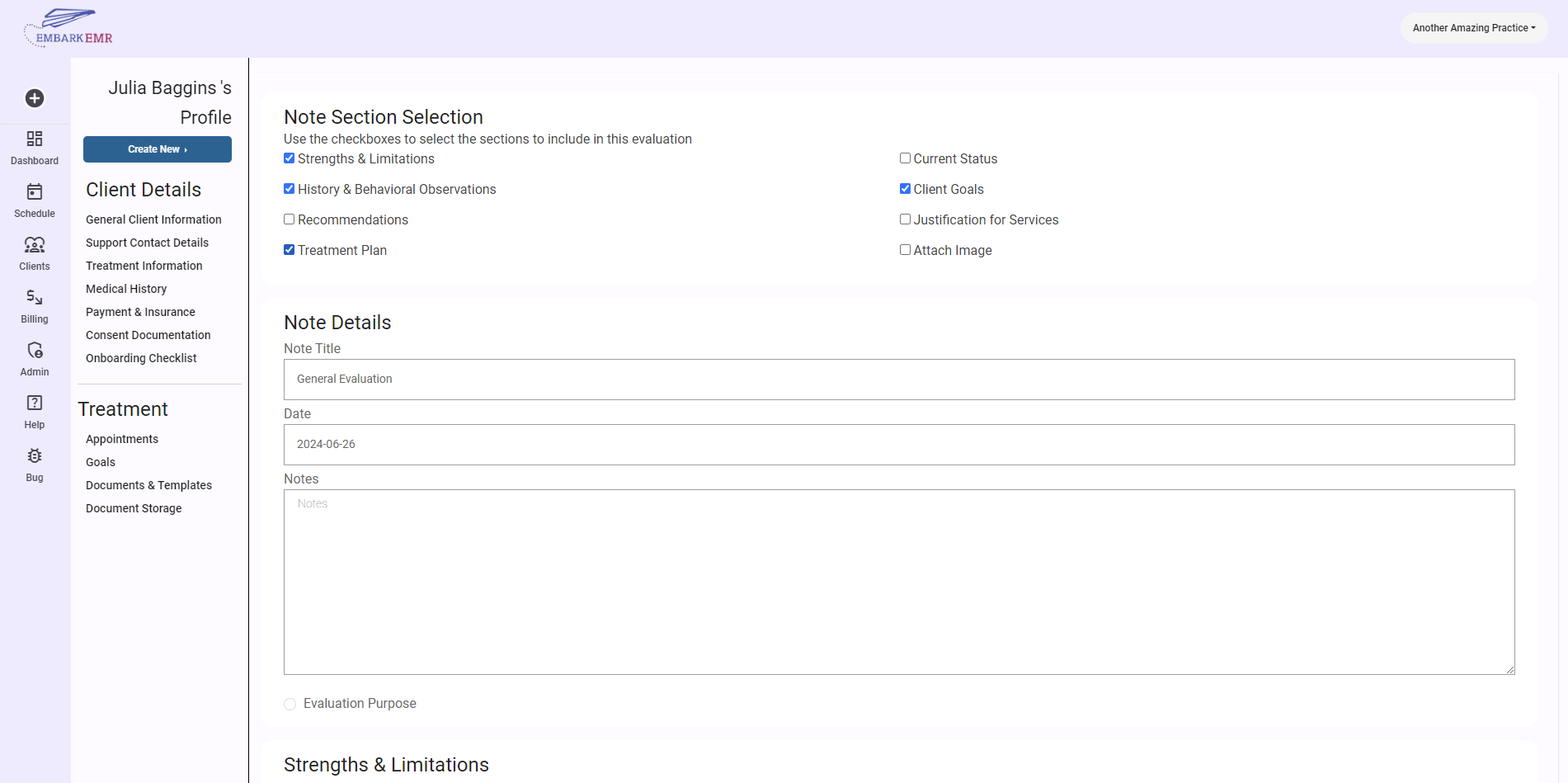
Set Up the Note:
- Once the dialogue box appears, fill out the necessary fields:
- Note Type: Select Progress or Discharge note as the note type
- Date: Specify the date of the note.
- Title: Provide a concise title that reflects the content of the note.
- Click “Add” to create the note template, which will now be saved and accessible under the “Documents & Templates” section.
- Once the dialogue box appears, fill out the necessary fields:
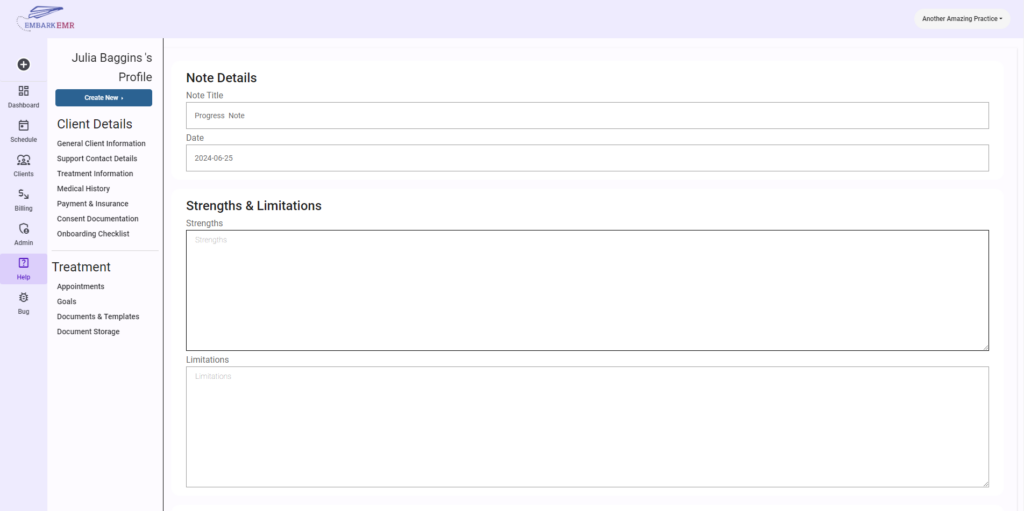
Filling Out the Progress/Discharge Note:
The progress/discharge note template includes several sections that allow you to detail the client’s current status and the progress made during their care:
- Strengths: Document the client’s key strengths or improvements observed during the treatment period.
- Limitations: Note any challenges or limitations the client is currently facing.
- Addressed Goals & Notes on Progress: List the goals that were addressed during the treatment period and provide notes on the progress made towards each goal.
- Add Specific Goals: Add goals from the client’s profile that you’ve addressed and detail the progress achieved.
- Summary: Provide a comprehensive summary of the client’s overall progress and current status.
- Planned Intervention: If applicable, describe any interventions planned for future sessions or after discharge.
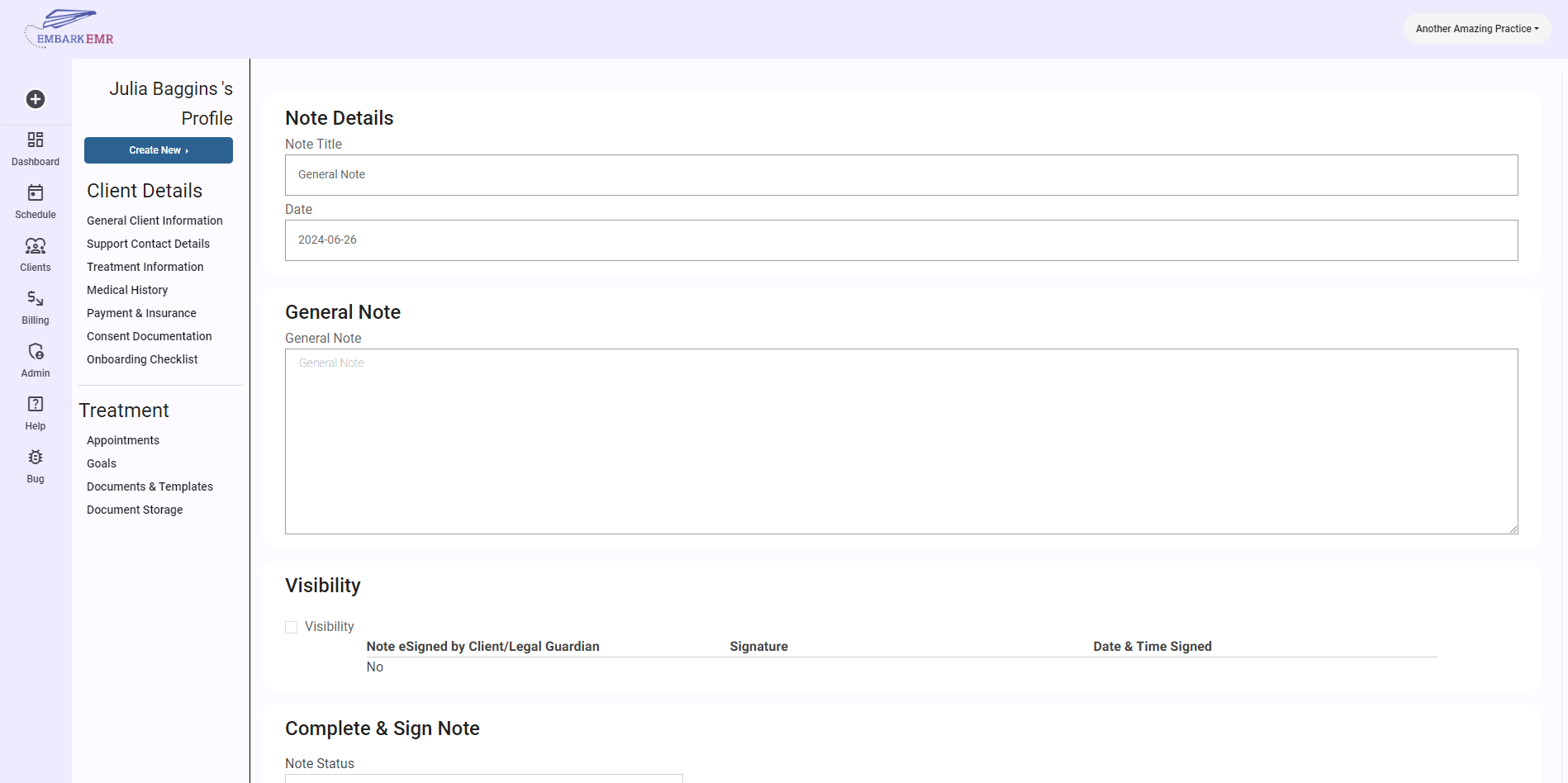
Finalizing and Sharing the Note:
- Release the Note to the Client: If you wish to share the note with the client via the client portal, check the option to release the note to the client. This makes the note accessible to the client for review.
- Request Client E-Signature: You can also opt to have the client electronically sign the note, providing an additional layer of verification and involvement.
- Provider E-Signature: As the final step, ensure that you, as the provider, electronically sign and date the note at the bottom. This action verifies the accuracy of the information and formally closes out the note.
Conclusion:
Creating and managing progress/discharge notes in Embark EMR is a streamlined process that enhances the documentation and communication of client care. These notes are not only crucial for tracking therapeutic outcomes but also provide essential insights during client transitions or discharge planning.
Tip: Regularly review and update progress/discharge notes to reflect any new information or changes in the client’s condition. This ensures that all involved parties, including subsequent caregivers, receive the most current and relevant information.